Health Risks of Dampness and Mold in Houses
Health Risks of Dampness and Mold in Houses
In 2004, the Institute of Medicine (IOM) of the National Academy of Sciences completed a review of the available scientific literature pertaining to the health consequences of building dampness and mold [1]. In 2009, the World Health Organization (WHO) completed a similar review [2]. Both organizations concluded that presence of dampness and mold in homes was associated with increases in several respiratory health effects but that the specific dampness-related agents causing the increases in respiratory health effects were unknown. Since the completion of work by these two organizations, several new articles with reviews of the literature have been published.
The key features and findings of these new reviews are summarized in Table 4. The detailed review by Mendell et al. [3] found that indoor dampness or mold, determined visually or via mold odor, was associated with increases in asthma exacerbation, cough, wheeze, upper respiratory symptoms, asthma development, shortness of breath, ever diagnosed asthma, respiratory infections, bronchitis, allergic rhinitis, and eczema. These conclusions largely mirror those of the prior reviews by the IOM and WHO, except for the findings that dampness and mold were associated with asthma development (onset of new asthma as opposed to just exacerbation of existing asthma) and with increased respiratory infections and bronchitis.
The IOM review, based on more limited data, had not concluded that dampness and mold were associated with asthma development, respiratory infections, or bronchitis. Mendell et al. [3] also reported suggestive evidence of increases in common cold and atopy (allergic sensitization, i.e., having an IgE type response to allergens) with visible dampness and mold, suggestive evidence of increased wheeze with higher ergosterol (a mold marker) in dust, and suggestive evidence of increased wheeze with higher endotoxin (primarily a marker of bacteria) in dust. The review by Park and Cox-Ganser [4] considered evidence from studies of dampness and mold in workplaces as well as in homes and had similar conclusions but also summarized evidence that two relatively rare lung diseases - hypersensitivity pneumonitis and sarcoidosis – increase in buildings with dampness and mold problems. The review by Tischer et al. [5] focused on children and concluded that visible mold and higher mold spore levels in homes were associated with increases in allergic respiratory health outcomes in children. Kanchongkittiphon et al. [6] considered only asthma exacerbation as an outcome. They concluded that dampness and dampness-related agents were casually related to asthma exacerbation in children and associated with asthma exacerbation in adults. They also found limited evidence of associations of asthma exacerbation with higher indoor concentrations of total fungi or fungi of the Penicillium genus.
The final row of Table 4 summarizes two papers that reviewed the health consequences of mold without an exclusive focus on the health risks of dampness and mold in buildings. Both articles find that there are relatively few health outcomes for which causal relationships between mold exposure and health has been proven. These few outcomes include mold infections and relatively rare lung diseases. These articles also indicate that there is minimal or no evidence of associations of mold with autoimmune diseases and sick building syndrome symptoms, although they do not provide a thorough discussion of associated data.
Table 4. Qualitative reviews published after 2009 of associations of dampness and mold in homes with health.
|
Issues Reviewed |
Key Findings |
Reference |
|
Associations of health with qualitative assessments of dampness or mold (such as report of visible mold) and with quantitative measurements of microbial agents |
Indoor dampness or mold determined visually or from mold odor was statistically significantly associated with increases in the following outcomes, generally with high consistency: asthma exacerbation, cough, wheeze, upper respiratory symptoms, asthma development, shortness of breath, ever diagnosed asthma, respiratory infections, bronchitis, allergic rhinitis, eczema. There was limited suggestive evidence of associations of dampness and mold with increased common cold and allergy/atopy. There was insufficient evidence to determine if dampness or mold were associated with lung function or hypersensitivity pneumonitis. There was limited suggestive evidence of an association of increased wheeze with higher ergosterol (a fungal marker) in dust. There was limited suggestive evidence of an association of increased wheeze with higher endotoxin (primarily a marker of bacteria) in dust. |
Mendell et al. 2011 [3] |
|
Associations of allergic and asthma health outcomes in children with visible mold, mold concentrations in air or dust, concentrations of markers of mold in homes |
Visible mold and mold spore levels were associated with increases in allergic respiratory health outcomes in children. There was less evidence of associations of other markers of molds or mold components with health. |
Tischer et al. 2011a [5] |
|
Associations of respiratory health outcomes with indoor dampness and mold at home and away from the home |
This review found evidence of associations of indoor dampness and mold or higher mold levels with development of asthma, asthma exacerbation, lower respiratory symptoms (such as cough, wheeze, shortness of breath), nasal and throat symptoms, and respiratory infections. There was also evidence that two relatively rare lung diseases - hypersensitivity pneumonitis and sarcoidosis – increase in buildings with dampness and mold problems. These findings were based on a review of studies of dampness and mold in both homes and workplaces.
|
Park and Cox-Ganser 2011 [4] |
|
Associations of indoor environmental exposures, including indoor dampness and mold, with exacerbation of asthma |
This review considered journal articles published between 2000 and 2013 and concluded: 1) there is a causal relationship between asthma exacerbation in children and indoor dampness or dampness-related agents; 2) asthma exacerbation in adults is associated with dampness or dampness-related agents; 3) there is limited or suggestive evidence of asthma exacerbation with indoor culturable Penicillium (a genus of fungi) and with indoor culturable total fungi. |
Kanchongkittiphon et al 2015 [6] |
|
Health effects of mold exposure |
These two reviews focus on the health consequences of mold without an exclusive focus on indoor dampness and mold. Both articles find that there are relatively few health outcomes for which causal relationships between mold exposure and health has been proven. These few outcomes include mold infections and relatively rare lung diseases. The article by Borgers et al. finds that reports of “toxic mold syndrome or toxic black mold have been shown to be no more than media hype and mass hysteria.” The article by Pettigrew et al. finds that there is basically no evidence that mold causes autoimmune diseases and suggests that mold is not likely a cause of sick building syndrome symptoms. |
At the time of the IOM’s review, there were no published meta-analyses of the relationships of dampness and mold with health. Meta-analyses statistically combine the results of multiple studies to develop central estimates of relationships of risk factors with health outcomes. Meta-analyses enable the results of multiple studies to be combined in a structured manner. Compared to typical literature reviews such as those in Table 4, the findings of meta-analyses are less subject to qualitative judgements.
Since the IOM’s review, the results of eight meta-analyses of dampness and mold in homes have been published and the associated papers are summarized in Table 5. In this table, statistically-significant central estimates are highlighted in bold font. These meta-analyses have generally found increases in respiratory symptoms (e.g., cough, wheeze, allergic rhinitis) and asthma diagnosis associated with visible dampness and mold with odds ratios generally in the range of 1.4 to 1.8, implying roughly 40% to 80% increases in health outcomes in homes with dampness and mold. The meta-analyses include few statistically significant associations of health outcomes with levels of mold spores or with concentrations of chemical markers of mold. Surprising, Tischer et al. [5] suggest a reduction in respiratory health effects associated with higher glucan levels (glucans are markers of fungi).
The key results of the first of these meta analyses [9] are depicted in Figure 1. This figure shows statistically significant associations of dampness and mold in homes with respiratory tract symptoms, cough, wheeze, current asthma, and ever having a diagnosis of asthma. It was estimated that these health outcomes increase by 30% to 50% in homes with dampness and mold. This analysis found a non-statistically significant approximately 30% increase in asthma development with dampness and mold. At the time of the analysis, results were available from only four studies of asthma development. The subsequent meta-analysis of Tischer et al. [10] also found small, approximately 10%, non-statistically-significant increases in development of asthma, when dampness and mold were present, except there was a statistically significant approximately 40% increase in asthma development for ages 0 – 2. However, the diagnosis of asthma can be uncertain in such young children. The various meta-analyses of Quansah et al. [11] which focused explicitly on asthma development, was able to utilize the results of 8 to 16 studies. In these analyses, there were statistically significant 30% to 70% increases in asthma development with four out of five indicators of dampness and mold.
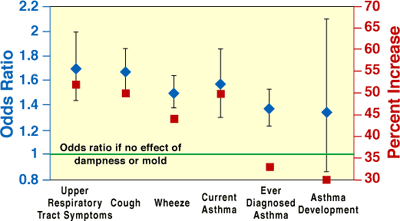
Figure 1. Results of analyses to quantify the average increases in health effects for occupants residing in homes with dampness or mold [9].
The second-listed meta-analysis of Fisk et al. [12] is the only one focusing on bronchitis and respiratory infections and the key results are shown in Figure 2. The analysis indicates statistically significant, approximately 30% to 40%, increases in bronchitis and various categories of respiratory infections among occupants of homes with dampness and mold. These analyses indicated statistically significant approximately 40% to 50% increases in bronchitis and various categories of respiratory infections in homes with dampness and mold.
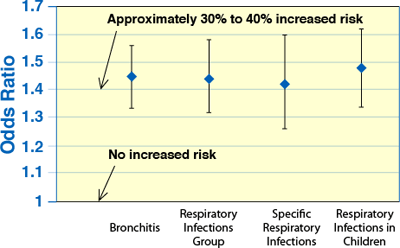
Figure 2. Results of analyses to quantify the average increases in respiratory infections and bronchitis for occupants residing in homes with dampness or mold [12].
The final meta-analysis in Table 5 [13] is unique in its focus on dampness and mold remediation. For adults, dampness remediation in homes was associated with reduced respiratory and asthma outcomes, including asthma medication use, often with odds ratios of approximately 0.6, indicating approximately a 40% decrease in health outcomes after remediation. Many of the findings were statistically significant.
Table 5. Meta analyses of associations of dampness and mold in homes with health.
|
Population(s); Number of Studies |
Risk Factors |
Control for confounding |
Health Outcomes and Estimate of Association with Dampness or Mold Expressed as Odds ratio or Effect Estimate (95% confidence interval) |
Reference |
|
Adults and children; Number of studies in analysis ranged from 4 for asthma development to 22 for wheeze |
Dampness, mold (visible mold or mold odor), or dampness and mold, in housing |
Required that individual studies controlled for confounding by age, gender, smoking, socio-economic status; Age > 3 for asthma development |
Upper respiratory symptom 1.70 (1.44 – 2.00) Cough, all ages 1.67 (1.49 – 1.86) Cough, Adults 1.52 (1.18 – 1.96) Cough, Children 1.75 (1.56 – 1.96) Wheeze, all ages 1.50 (1.38 – 1.64) Wheeze, adults 1.39 (1.04 – 1.85) Wheeze, children 1.53 (1.39 – 1.68) Ever diagnosed with asthma 1.37 (1.23 – 1.53) Asthma development 1.34 (0.86 – 2.10) |
Fisk et al 2007 [9] |
|
58,000 children age 6 -12; 12 studies in Russia, North America, Europe |
Visible mold in home |
Controlled for age, sex, maternal education, paternal education, nationality, crowding, unvented combustion heating, smoker in house, birth order, ever had a pet |
Wheeze in past 12 months 1.43 (1.36 – 1.49) Ever asthma 1.35 (1.20 – 1.51) Bronchitis in past 12 months 1.38 ( 1.29 – 1.47) Nocturnal dry cough in past 12 months 1.30 (1.22 – 1.39) Morning cough 1.50 (1.31 – 1.73) Sensitivity to inhaled allergens 1.33 (1.23 – 1.44) Ever hay fever 1.35 (1.18 – 1.53) Woken by wheeze in past 12 months 1.49 (1.28 – 1.74) |
Antova et al. 2008 [14] |
|
Children and adults; 13 to 19 studies with 57 to 20,059 subjects per study |
Any of dampness, water damage, visible mold, mold odor, history of flooding in home |
For results reported in this table, individual studies controlled for age, gender, smoking, socio-economic status
|
Acute or chronic bronchitis 1.45 (1.32 – 1.59) Respiratory infection All ages 1.44 (1.31 – 1.59) Children 1.48 (1.33 – 1.65) Adults 1.49 (1.14 – 1.95) Respiratory infection excluding otitis media 1.40 (1.29 – 1.52) Respiratory infection excluding common cold and non-specific infections 1.50 (1.32 – 1.70) Common cold or acute upper respiratory infection 1.38 (1.13 – 1.65) |
Fisk et al. 2010 [12] |
|
Children; 21 studies for asthma, 19 studies for wheeze, 10 studies for allergic rhinitis |
Visible mold, mold concentrations in air or dust; concentrations markers of mold; all at home |
Not described |
For visible mold: Doctor-diagnosed asthma 1.49 (1.28 – 1.72) Wheeze 1.68 (1.48 – 1.90) Allergic rhinitis 1.39 ( 1.28 – 1.51)
For concentrations of mold spores or of markers of mold in air or dust, there were fewer significant findings. Higher mold spore levels were associated with increased wheeze and asthma in young children; however, there was a tendency for lower risks of allergic health outcomes with higher concentrations on markers of molds, such as glucans. |
Tischer et al. 2011a [5] |
|
31,742 children; 8 birth cohorts in Europe |
Visible dampness or mold in home during first 2 years of life |
Controlled for gender, parental atopy, parental education, maternal smoking during pregnancy, smoke at home in 1st two years of life, breast feeding, day care |
Asthma during age 0 – 2 1.39 (1.05 – 1.95) Asthma during age 6 – 8 1.09 (0.90 – 1.32) Asthma ever during age 3 – 10 1.10 (0.90 – 1.34) Allergic rhinitis during age 6 – 8 1.12 (1.02 – 1.23) Allergic rhinitis during age 3 – 10 1.18 (1.09 – 1.28) Sensitization to airborne allergens during age 6 – 8 1.05 (0.89 – 1.24) |
Tischer et al 2011b [10] |
|
Children or adults; 8 to 16 studies depending upon analysis |
Combinations of water damage, damp stains or other dampness indicators, visible mold, mold odor |
No described |
For onset of asthma: Any dampness or mold indicator 1.50 (1.25 – 1.80) Water damage:1.12 (0.98 – 1.27) Dampness indicators 1.32 (1.12 – 1.57) Visible mold 1.29 (1.04 – 1.60) Mold odor 1.73 (1.19 – 2.50) |
Jaakkola et al. 2013 [15] |
|
Children or adults; 31 studies |
Any of water damage, damp stains or other dampness indicators, visible mold, mold odor in home |
Not described |
Rhinitis Any risk factor 2.08 (1.56 – 2.76) Water damage 1.71 (0.69 – 4.22) Damp stains 1.82 (1.34 – 2.46) Visible mold 1.82 (1.56 – 2.12) Mold odor 2.18 (1.76 – 2.71) Allergic rhinitis Any risk factor 1.52 (1.29 – 1.80) Water damage 1.46 (0.98 – 2.19) Damp stains 1.50 (1.38 – 1.62) Visible mold 1.51 (1.39 – 1.64) Mold odor 1.87 (0.95 – 3.68) Rhinoconjunctivitis Damp stains or visible mold 1.68 (1.41 – 2.00) Damp stains 1.67 (1.41 – 1.98) Visible mold 1.66 (1.27 – 2.18) |
Jaakkola et al 2013 [16] |
|
Children and adults in buildings that received dampness remediation; 12 total studies but as few as 2 studies per analysis |
Dampness remediations |
Intervention study designs controls for personal/ demographic factors and many building characteristics |
Reported results are too numerous for replication in this table. The main findings were:
|
Sauni et al. 2015 [13] |
In summary, based on reviews of a large number of quality studies and based on meta-analyses of study findings, indoor dampness or mold, determined visually or via mold odor, is associated with increases in asthma exacerbation, cough, wheeze, upper respiratory symptoms, asthma development, shortness of breath, ever diagnosed asthma, respiratory infections, bronchitis, allergic rhinitis, and eczema. The odds ratios resulting from meta-analyses often indicate 30% to 70% increases in the prevalence rates of health effects in homes with dampness and mold. However, research has not clearly identified the specific dampness-related agents causing the increases in respiratory health effects.
Health Risks of Dampness and Mold in Workplaces
Substantial research has been completed to investigate the associations of adverse health effects with dampness and mold in workplaces. (For information on the health consequences of dampness and mold in schools, see the section of this web site on IAQ in Schools). Sixteen studies published in 18 peer-reviewed journal articles were identified and key study features and findings are provided in Table 6. Five studies [17-21] report statistically significant increases in asthma health outcomes (asthma diagnosis, asthma exacerbation, or asthma onset) in buildings with visible dampness or mold or mold odor. A sixth study reported in three papers [22-24] found statistically significant increases in asthma outcomes in buildings with damp concrete causing an increase in airborne concentration of the chemical 2-ethyl-1-hexanol from degradation of PVC flooring placed on that concrete. Importantly, three studies [18-20] found dampness and mold associated with statistically significant increases in asthma onset (development of new asthma). The study of Jaakkola et al. [18], which has the strongest design of these three studies, reports approximately a 50% increase in onset of asthma in work places with dampness and mold. Ten out of 11 studies with health symptoms as outcomes reported a statistically significant increase in at least one type of health symptom with increased indications of dampness and mold and in many instances the prevalence of symptoms more than doubled. In most studies, some symptoms were not associated with dampness and mold. The dampness-related risk factors associated with increased health symptoms varied among these 10 studies. For three studies, symptoms increased with increased visible dampness or mold or mold odor [17, 25, 26]. In one study, increased symptoms were associated with dampness in the heating, ventilating, and air conditioning systems [27]. In one study, ultraviolet irradiation of the wet cooling coils (which reduces fungal and bacterial growth) reduced symptoms [28]. One study found symptoms increasing with higher levels of mold in chair dust but not air [29] while another study reported symptoms increasing with increased molds in floor dust but not chair dust [30]. Finally, in one study [22-24] symptoms increased in buildings with damp concrete that caused degradation of PVC flooring and increases of airborne levels of 2-ethyl-1-hexanol. One study [31] failed to find statistically significant increases in health outcomes with dampness and mold, although most health symptoms increased non-significantly and there was a statistically significant increase in workdays lost to respiratory symptoms. Most of the studies had a cross sectional design that can identify associations but not provide proof of causal relationships, although most studies controlled for a substantial set of potential confounding factors. The study of Jaakkola et al. [18] had a stronger case-control design and the study of Menzies et al. [28] was a very strong blinded crossover intervention study. In summary, the published literature indicates an association of asthma and other respiratory health outcomes in damp or moldy workplaces.
Table 6: Key features and results of research on dampness and health in workplaces other than schools.
|
Author Study Type |
Buildings Subjects |
Dampness or Mold related Risk Factors |
Confounders Controlled |
Key findings |
|
Chao et al. 2003 [29] Cross sectional |
98 adults in 21 offices in 4 buildings |
Mold spore count in air, floor and chair dust. Principal component analysis factors based on mold. |
Personal and job factors, temperature, humidity, carbon dioxide, dust load on floor and chairs |
With higher chair mold levels there were statistically significant increases in upper respiratory symptoms [OR=1.35, CI = 1.07 – 1.70], and non-specific symptoms [OR = 1.87, CI = 1.11- 3.15], but not with eye symptoms. Airborne mold levels were not significantly associated with symptoms in the final models that controlled for confounding by other factors |
|
Cox-Ganser et al. 2005 [17] Main study was cross sectional.
Supplemental study compares outcome prevalence in study with reference populations |
Main study- 888 adults from 1 damp building. Supplemental study- 248 adults in high respiratory symptom, vs. low respiratory symptom, vs. no respiratory symptom groups |
Damp building |
Smoking |
Main Study: In study population of 888 adults relative to subjects of NHANES survey, there were statistically significant elevations in ever asthma [OR = 2.2, CI = 1.9 – 2.6], current asthma [OR=2.4, CI=2.0 – 3.0], adult onset asthma [OR=3.3, CI=2.7 – 4.0], wheeze [OR=2.5, CI=2.2 – 2.8], nasal symptoms [OR=1.5, CI=1.4 – 1.6], eye symptoms [OR=1.6, CI=1.4 – 1.7]. In study population relative to population in 100 representative office buildings, there were statistically significant elevations in wheeze [OR=2.9, CI=2.2 – 3.7], cough [OR=2.7, CI=2.3 – 3.2], tight chest [OR=4.7, CI=3.8 – 5.7], shortness of breath [OR=4.6, CI=3.7 – 5.7], 7-fold more adult onset asthma after starting work in building. Supplementary study: Objective tests confirmed more abnormal lung function and breathing medication use in subjects with more self-reported symptoms. |
|
Jaakkola et al. 2002 [18]
Case control
|
512 adults with new asthma and 912 control adults without asthma |
Water damage, visible dampness, visible mold, mold odor |
Sex, age, parental atopy or asthma, education level as indicator of socio economic status, smoking, environmental tobacco smoke, dampness at home, pets, occupational exposures to sensitizers, dusts, or fumes |
An increased risk of new asthma (development of the disease of asthma) was associated with visible mold or mold odor at work [OR=1.54, CI=1.01 – 2.32]. There were no statistically significant associations of new asthma with water damage or damp stains without visible mold or mold odor. |
|
Jarvis and Morey 2001 [32]
Before versus after evacuation from an office building with planned mold remediation |
488 occupants of mold remediated building and 122 people who had moved from this buildings to another building, reference population was 261 occupants in non-remediated office building |
Before versus after evacuation from an office building with planned mold remediation |
Not specified |
There were statistically significant 32% to 50% decreases in throat, nose, eye, and headache symptoms after evacuation from the damp office building, but no statistically significant changes in chest tightness, shortness of breath, cough, or wheeze. |
|
Karvala et al. 2010 [19]
Cross sectional (analysis of case histories) |
694 adult patients with respiratory symptoms who had been exposed to molds at work |
Date of first exposure to moisture damaged workplace, level of mold exposure based on extent of mold damage and levels of airborne molds |
Patients with residential moisture damage were excluded, |
There was a statistically significant association of high level of mold exposure at work with development of probable work-related asthma although the odds ratio and confidence limits were not reported |
|
Karvala et al. 2011 [20]
Longitudinal |
483 patients initially with asthma-like symptoms related to damp work places but without asthma, 62 of which developed asthma 3-12 years later |
Continued exposure to damp or mold workplace environment, dampness remediation at work |
Age, gender, atopic history, smoking habits |
Continued exposure to damp or mold in workplace environment was associated with increased risk of developing asthma [OR=4.6, CI=1.8 – 11.6] The risk of developing asthma was lower and not statistically significant if there had been a dampness/mold remediation at work [OR=2.0, CI = 0.7 – 5.40] suggesting that mold remediation at work reduced the risk of developing asthma |
|
Kim et al. 2016 [21]
Cross sectional |
1356 working adults who reported that they have or ever had asthma |
Self-reported dampness or mold at work (visible water damage, visible mold, mold odor) |
Gender, age, smoking status, second hand smoke, history of allergy |
Exposure to workplace dampness or mold was associated with increased asthma exacerbation [OR=1.79, CI=1.19 – 2.67] |
|
Mendell et al. 2003 [27]
Cross sectional |
2345 adults in 80 complaint office buildings in U.S. |
Water in outdoor air intake, moist internal duct insulation, poor drain pan drainage, water damage in workspace. |
Age, sex, smoking status, asthma status |
Poor cooling coil drain pan drainage was associated with at least 3 of the following symptoms: Wheeze, shortness of breath, tight chest, cough [OR=2.6, CI=1.3 – 5.2] Poor cooling coil drain pan drainage was associated with having all three of wheeze, shortness of breath, cough [OR=2.8, CI = 1.1 – 5.2] |
|
Menzies et al 1998 [33] Cross sectional |
214 adults in 6 office buildings |
Mold spore levels in air, floor dust & HVAC supply air, Indoor minus outdoor humidity |
Age, sex, atopic status, smoking; temperature, humidity, carbon dioxide, total volatile organic compounds, total suspended particulates |
For workers with respiratory symptoms versus those without symptoms, the probability of detectable Alternaria (a mold) in office air was significantly elevated [OR=4.2, CI=1.1 – 16.2]; For workers with symptoms, there was a significantly higher indoor air minus outdoor air humidity level (p < 0.010) |
|
Menzies et al 2003 [28] Blinded crossover intervention study |
771 adults in 3 office buildings |
Ultraviolet germicidal irradiation of cooling coils as an intervention |
The within-person analysis controls personal factors, temperature, humidity, carbon dioxide, nitrogen dioxide, ozone. |
Operation of ultraviolet germicidal system was associated with statistically significant reductions in symptoms as follows: Any symptom [OR=0.8, CI=0.7 - 0.99]; Mucosal symptom [OR=0.7, CI=0.6 - 0.9]; Respiratory symptom [OR=0.6, CI=0.4 - 0.9] Operation of ultraviolet germicidal system was associated with a non-significant reduction in musculoskeletal symptoms [OR=0.8, CI=0.6 -1.1] |
|
Norback et al. 2000 [22]
Nordstrom et al. 1999 [23]
Wieslander et al. 1999 [24] Cross sectional |
87 or 88 staff (depending on analysis) from four geriatric hospitals |
Dampness in concrete floor and associated elevated airborne concentrations of 2-ethyl-1-hexanol from degradation of a plasticizer in the PVC floor covering of the concrete |
Age, sex, atopy, dampness at home
Age, sex, tobacco smoking, atopy, psychosocial work environment, building age
Age, sex, smoking habits, atopy, psychosocial index
|
In the two buildings with floor dampness- and elevated airborne concentrations of 2 –ethyl-1-hexanol, asthma symptoms were increased [OR 8.6, CI 1.3 – 56.7]
Eye symptoms increased, not statistically significantly [OR 1.72, CI 0.89 – 3.32] Nasal symptoms increased [OR 1.13, CI 1.04 – 1.24] Throat symptoms increased [OR1.15, CI 1.05 – 1.26] General symptoms increased [OR 1.16, CI 1.07 – 1.25]* There was no association with facial skin symptoms
Weekly eye symptoms in past 3 months increased [OR= 1.29, CI = 1.15 – 1.45] Weekly nose symptoms in past 3 months increased [OR= 1.10, CI = 1.02 – 1.18] There was a statistically significant decrease in tear film break up time and increase in nasal lysosome (a marker of inflammation) but no statistically significant change in nasal openness |
|
Park et al. 2006 [30] Cross sectional |
888 adults in one 20-story water damaged building |
Fungi and endotoxin concentration in floor and chair dust ranked as low, medium, and high for each. |
Age, gender, race, smoking, duration of occupancy. |
In groups with highest versus lowest fungal concentrations in floor dust, there were statistically significant increases in lower respiratory symptoms [OR=1.7, CI=1.02-2.77 to OR=2.4, CI =1.29-4.59]; throat irritation [OR=1.7, CI=1.06-2.82]; rash/itchy skin [OR 3.0, CI=1.47-6.19]. Endotoxin increased associations of fungi on respiratory symptom, .i.e., presence of both endotoxin and fungi was associated with greater increase than their added individual effects. |
|
Sahakian et al 2009 [31]
Cross sectional |
1396 office workers |
Self-reported workplace dampness defined as visible mold, moldy/musty odor, or water damage; workplace air conditioning |
Age, gender, smoking status, race, education, household income, geographic region, seasonal allergies, flu shot in prior year, obesity |
With workplace dampness: Respiratory infections of various types increased or decreased but the changes were not statistically significant Work related nasal symptoms, lower respiratory symptoms, work related lower respiratory symptoms, constitutional symptoms, and asthma increased but the increases were not statistically significant Nasal symptoms decreased but the decrease was not statistically significant Workdays lost to respiratory symptoms increased [PR=1.30, CI=1.02 – 1.65] There were no statistically significant changes in visits to doctors |
|
Wan et al. 1999 [25] Cross sectional |
1113 adults in 9 air conditioned office buildings |
Visible mold or mildew, signs of water damage, flooding. |
Age, sex, atopy, job satisfaction, perceived ventilation. |
Skin symptoms increased in buildings with mold [OR=2.97, CI=1.52 – 5.82], increased with water damage [OR=3.36, CI=1.70 – 6.63], and increased with flooding [OR=2.6, CI=1.19 – 2.56]. Headache increased with mold [OR=1.61, CI 1.01 – 2.56] There were non-statistically significant increases in many other symptoms including shortness of breath with mold, water damage, or flooding. |
|
Wan et al 1999b [26] Cross sectional |
109 adults in 8 office and 8 daycare buildings |
Visible mold, water damage, flooding. Mold and bacteria colony forming units, & endotoxin in air. b-1,3-glucan (a marker of mold) in air .
|
Sex, ventilation rate, type of building |
Shortness of breath, but none of nine other symptoms, was statistically significantly increased in buildings with mold [OR=20.75, CI=2.23 – 193.5] There were no statistically significant associations of water damage or flooding with symptoms of any type. |
|
Zhang et al. 2012 [34]
Longitudinal |
429 adults in workplace buildings |
Floor dampness, dampness or molds, moldy odor, at baseline and 10 years later |
Age, sex, atopy, smoking, education level |
There were no statistically significant associations of dampness and mold at baseline with subsequent new sick building syndrome symptoms. Floor dampness in the final year was associated with onset of mucosal symptoms [OR=4.46, CI = 1.39 – 14.35]. Floor dampness at any workplace during the 10 year period was associated with onset of mucosal symptoms [OR= 2.43, CI= 1.05 – 5.64] There were non-statistically significant increases in onset of general and mucosal symptoms with other indicators of dampness and mold. There were decreased remissions of symptoms present at baseline in buildings with dampness and mold indicators, but only one decrease in remission was statistically significant with decreased remission of general symptoms in buildings repaired because of dampness [OR = 0.21, CI = 0.07 – 0.70]. There was evidence, sometimes statistically significant, that dampness and mold was associated with increased biomarkers of inflammation and increased bronchial responsiveness |
Key to table: CI = 95% confidence interval; OR = odds ratio; PR = prevalence ratio *In this study, general symptoms were not defined but the term usually refers to headache, fatigue, dizziness, difficulty concentrating.
Health Risks of Dampness and Mold in Schools
A detailed discussion of the health risks of dampness and mold in schools is provided in the section of this web site on IAQ in Schools. The relatively consistent findings of a substantial number of quality studies indicate that there is an association of dampness and mold in schools with increased respiratory health symptoms, such as cough or wheeze, among occupants of the schools. Visible dampness and mold or mold odor are more clearly associated with symptoms than are higher levels of measured mold in air or dust. Objective health measures are, however, less consistently associated with dampness and mold in schools. Overall, these findings mirror those available from a larger body of research on dampness and mold in homes.
Health Risks of Dust Mite Allergens
Research has clearly demonstrated that dust mite allergen increases the risk of various health effects [35]. Nearly all of this research has been performed in houses. Where concentrations of mite allergen in house dust are greater than approximately 2 micrograms allergen per gram of dust, susceptible people have a much higher risk of becoming sensitized to (i.e., have an allergic response to) dust mite allergen [35, 36]. Those who are sensitized to dust mite allergen have a several-fold increased risk of asthma [35]. Mite allergens exacerbate allergic rhinitis (allergen-caused inflammation of the nasal tissues causing runny nose or congestion) and atopic dermatitis (allergen-caused inflammation of the skin resulting in rash and itching) [37]. A National Academy of Science committee concluded that the evidence was sufficient to conclude that dust mite allergen caused development of the disease of asthma and caused exacerbation of asthma in those with asthma [35].
Given the strong evidence of the health risks of dust mite allergens, there have been many studies of the health benefits for various interventions designed to reduce dust mite allergen exposures. Three health studies reviewed included measures designed to reduce indoor humidity [38-40]. Two of three studies [39, 40] reported statistically significant health benefits as summarized in Table 3. In one of these studies the health benefits could have resulted from changes in bedding, removal of carpeting, and improved cleaning which were implemented at the same time as ventilation to reduce humidity [39]. In another of these studies [40], the subjects moved to new houses which could have resulted in many environmental changes other than a reduction in indoor humidity; thus, the health benefits cannot be clearly attributed to reduced indoor humidity and associated reductions in dust mites. Given the small amount of data and that several other studies were unable to significantly reduce indoor humidity or dust mite levels [41-43], we must conclude that the health benefits of humidity reduction interventions designed to reduce indoor dust mites are not well documented.
In another section of this website, two studies are noted that found higher levels of dust mite allergen in homes with evaporative cooling [22, 29]. Two other studies have investigated the association of evaporative cooling of homes with health outcomes. Aldous et al. [44] followed lower respiratory illness in the first year of life of 936 infants from Tucson and reported a substantial increase in lower respiratory illness with wheeze in infants who resided in homes with evaporative cooling, after controlling for various potential confounding factors. The odds ratio was 1.8 with a 95% confidence interval of 1.1 to 3.0, so the findings were statistically significant. Prasad et al. [45] evaluated 190 patients, age 1-42, for sensitization to allergens. Thirty four percent of patients from homes with evaporative cooling were sensitized to dust mite allergen, compared to 18% from homes without evaporative cooling. In addition, 42% of patients from homes with evaporative cooling were sensitized to at least one mold allergen, compared to 19% from homes without evaporative coolers. Both findings were statistically significant.
Health Risks of Mycotoxins from Damp Buildings
Some molds can produce highly toxic chemicals called mycotoxins under some growth conditions. Some bacteria can also produce toxic chemicals. The potential health effects of mycotoxins have been reviewed by a committee of the National Academy of Sciences, Institute of Medicine [1]. These mycotoxins may be constituents of the particles released into indoor air. Studies with exposures to living cells and animals indicate that some mycotoxins are very potent. Documented or suspected health effects from mycotoxins in these studies include tremors, loss of coordination, lesions, increased levels of chemicals linked to inflammation, immune system suppression, cell death, and animal death. However, it is not known whether the indoor air concentrations of mycotoxins caused by microbial growth in damp buildings become high enough to cause any of these health effects.
In 1997, the toxins that can be produced by a type of mold called Stachybotrys chartarum became the suspected source of a cluster of pulmonary hemorrhages (bleeding in the lungs) and deaths among infants in Cleveland [46, 47]. These findings were broadly publicized and became controversial [48]. A task force was convened by the Centers for Disease Control and Prevention to review the evidence, noted shortcomings in the data collection and analyses, and concluded that Stachybotrys chartarum was not a definitive cause of pulmonary hemorrhage [48]. The Institute of Medicine committee referenced above also reviewed the related literature and concluded that there was inadequate or insufficient evidence to determine whether Stachybotrys chartarum or dampness in buildings causes pulmonary hemorrhage.
The health effects of indoor mycotoxins remains a controversial topic.
Health Risks of Microbial and Non-Microbial Gaseous Chemicals associated with Indoor Dampness
The health risk of the increases in microbial and non-microbial indoor gas-phase chemicals in indoor air from building dampness are not well understood. Some of the microbial volatile organic compounds (microbial VOCs or MVOCs) released by molds are sources of odors [1]. Some microbial VOCs are known to be irritating if concentrations are sufficient but it is not known whether microbial contamination in buildings can lead to sufficient indoor air concentrations of these VOCs to cause irritation [1].
As noted above, high humidity or wetted building materials can lead to increased rates of release of formaldehyde – a volatile organic compound – into indoor air. The significant health risks of formaldehyde are discussed in another section of this web site; however, we identified no direct studies of the increased risks from formaldehyde in damp buildings. Alcohols and degradation products from the softening agents used in many plastics can also be released when floor products containing polyvinyl chloride (PVC) are underlain by damp concrete. In several case studies, these chemicals have been cited as a source of odors and irritation [1]; however, no extensive or systematic studies of the health effects of these chemicals were identified.
Health-Related Costs of Dampness and Mold
Two papers were identified that have estimated the health related costs of dampness and mold in buildings and both consider only dampness and mold in homes within the United States. Mudarri and Fisk [49] estimated that 21% (range 12% to 29%) of current asthma in the U.S. was attributable to dampness and mold which corresponded in 2004 to 4.6 million (2.7 to 6.3 million) cases of current asthma. The associated annual cost was $3.5 billion (range $2.1 to $4.8 billion). In a more recent analysis Mudarri [50] estimated that dampness and mold in U.S. homes in the year 2014 cost $3.7 ($2.3 to $4.7) billion for allergic rhinitis, $1.9 ($1.1 to $2.3) billion for acute bronchitis, $15.1 ($9.4 to $20.6) billion for asthma morbidity, and $1.7 ($0.4 to $4.5) billion for asthma-caused mortality.
References:
3. Mendell, M.J., et al., Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect, 2011. 119(6): p. 748-756. https://dx.doi.org/10.1289/ehp.1002410.
4. Park, J.H. and J.M. Cox-Ganser, Mold exposure and respiratory health in damp indoor environments. Front Biosci (Elite Ed), 2011. 3: p. 757-71. https://dx.doi.org/10.2741/e284.
5. Tischer, C., C.M. Chen, and J. Heinrich, Association between domestic mould and mould components, and asthma and allergy in children: a systematic review. Eur Respir J, 2011. 38(4): p. 812-24. https://dx.doi.org/10.1183/09031936.00184010.
6. Kanchongkittiphon, W., et al., Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environmental health perspectives, 2015. 123(1): p. 6. https://dx.doi.org/10.1289/ehp.1307922.
7. Pettigrew, H.D., et al., Mold and human health: separating the wheat from the chaff. Clin Rev Allergy Immunol, 2010. 38(2-3): p. 148-55. https://dx.doi.org/10.1007/s12016-009-8175-5.
8. Borchers, A.T., C. Chang, and M. Eric Gershwin, Mold and Human Health: a Reality Check. Clin Rev Allergy Immunol, 2017. 52(3): p. 305-322. https://dx.doi.org/10.1007/s12016-017-8601-z.
9. Fisk, W.J., Q. Lei-Gomez, and M.J. Mendell, Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air., 2007. 17(4): p. 284-295. https://dx.doi.org/10.1111/j.1600-0668.2007.00475.x.
10. Tischer, C.G., et al., Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy, 2011. 66(12): p. 1570-9. https://dx.doi.org/10.1111/j.1398-9995.2011.02712.x.
11. Quansah, R., et al., Residential dampness and molds and the risk of developing asthma: a systematic review and meta-analysis. PLoS One, 2012. 7(11): p. e47526. https://dx.doi.org/10.1371/journal.pone.0047526.
12. Fisk, W.J., E. Eliseeva, and M.J. Mendell, Association of residential dampness and mold with respiratory tract infections and bronchitis: a meta-analysis. Environmental Health, 2010. 9:72. https://dx.doi.org/10.1186/1476-069X-9-72.
13. Sauni, R., et al., Remediating buildings damaged by dampness and mould for preventing or reducing respiratory tract symptoms, infections and asthma. Cochrane Database Syst Rev, 2015(2): p. Cd007897. https://dx.doi.org/10.1002/14651858.CD007897.pub3.
14. Antova, T., et al., Exposure to indoor mould and children's respiratory health in the PATY study. J Epidemiol Community Health, 2008. 62(8): p. 708-14. https://dx.doi.org/10.1136/jech.2007.065896.
16. Jaakkola, M.S., et al., Association of indoor dampness and molds with rhinitis risk: a systematic review and meta-analysis. J Allergy Clin Immunol, 2013. 132(5): p. 1099-1110.e18. https://dx.doi.org/10.1016/j.jaci.2013.07.028.
17. Cox-Ganser, J.M., et al., Respiratory morbidity in office workers in a water-damaged building. Environ Health Perspect, 2005. 113(4): p. 485-90. https://dx.doi.org/10.1289/ehp.7559.
19. Karvala, K., et al., New-onset adult asthma in relation to damp and moldy workplaces. Int Arch Occup Environ Health, 2010. 83(8): p. 855-65. https://dx.doi.org/10.1007/s00420-010-0507-5.
20. Karvala, K., et al., Prolonged exposure to damp and moldy workplaces and new-onset asthma. Int Arch Occup Environ Health, 2011. 84(7): p. 713-21. https://dx.doi.org/10.1007/s00420-011-0677-9.
21. Kim, J.L., et al., Impact of occupational exposures on exacerbation of asthma: a population-based asthma cohort study. BMC Pulm Med, 2016. 16(1): p. 148. https://dx.doi.org/10.1186/s12890-016-0306-1.
23. Nordstrom, K., et al., The effect of building dampness and type of building on eye, nose and throat symptoms in Swedish hospitals. Journal of Environmental Medicine, 1999. 1: p. 127-135. https://dx.doi.org/10.1002/1099-1301.
24. Wieslander, G., et al., Nasal and ocular symptoms, tear film stability and biomarkers in nasal lavage, in relation to building-dampness and building design in hospitals. Int Arch Occup Environ Health, 1999. 72(7): p. 451-61. https://dx.doi.org/10.1007/s004200050398.
26. Wan, G.H. and C.S. Li, Indoor endotoxin and glucan in association with airway inflammation and systemic symptoms. Arch Environ Health, 1999. 54(3): p. 172-9. https://dx.doi.org/10.1080/00039899909602256.
27. Mendell, M.J., et al., Environmental risk factors and work-related lower respiratory symptoms in 80 office buildings: an exploratory analysis of NIOSH data. Am J Ind Med, 2003. 43(6): p. 630-41. https://dx.doi.org/10.1002/ajim.10211.
28. Menzies, D., et al., Effect of ultraviolet germicidal lights installed in office ventilation systems on workers' health and wellbeing: double-blind multiple crossover trial. Lancet, 2003. 362(9398): p. 1785-91. https://dx.doi.org/10.1016/S0140-6736(03)14897-0.
29. Chao, H.J., et al., The work environment and workers' health in four large office buildings. Environ Health Perspect, 2003. 111(9): p. 1242-8. https://dx.doi.org/10.1289/ehp.5697.
30. Park, J.H., et al., Fungal and endotoxin measurements in dust associated with respiratory symptoms in a water-damaged office building. Indoor Air, 2006. 16(3): p. 192-203. https://dx.doi.org/10.1111/j.1600-0668.2005.00415.x.
31. Sahakian, N., J.H. Park, and J. Cox-Ganser, Respiratory morbidity and medical visits associated with dampness and air-conditioning in offices and homes. Indoor Air, 2009. 19(1): p. 58-67. https://dx.doi.org/10.1111/j.1600-0668.2008.00561.x.
32. Jarvis, J.Q. and P.R. Morey, Allergic respiratory disease and fungal remediation in a building in a subtropical climate. Applied Occupational and Environmental Hygiene, 2001. 16(3): p. 380-388. https://dx.doi.org/10.1080/10473220117482.
33. Menzies, D., et al., Aeroallergens and work-related respiratory symptoms among office workers. J Allergy Clin Immunol, 1998. 101(1 Pt 1): p. 38-44. https://dx.doi.org/10.1016/S0091-6749(98)70191-5.
34. Zhang, X., et al., Dampness and moulds in workplace buildings: associations with incidence and remission of sick building syndrome (SBS) and biomarkers of inflammation in a 10 year follow-up study. Sci Total Environ, 2012. 430: p. 75-81. https://dx.doi.org/10.1016/j.scitotenv.2012.04.040.
37. Arlian, L.G. and T.A. Platts-Mills, The biology of dust mites and the remediation of mite allergens in allergic disease. J Allergy Clin Immunol, 2001. 107(3 Suppl): p. S406-13. https://dx.doi.org/10.1067/mai.2001.113670.
38. Warner, J.A., et al., Mechanical ventilation and high-efficiency vacuum cleaning: A combined strategy of mite and mite allergen reduction in the control of mite-sensitive asthma. J Allergy Clin Immunol, 2000. 105(1 Pt 1): p. 75-82. https://dx.doi.org/10.1016/s0091-6749(00)90181-7.
39. Korsgaard, J., Preventive measures in mite asthma. A controlled trial. Allergy, 1983. 38(2): p. 93-102. https://dx.doi.org/10.1111/j.1398-9995.1983.tb01592.x.
40. Harving, H., J. Korsgaard, and R. Dahl, Clinical efficacy of reduction in house-dust mite exposure in specially designed, mechanically ventilated "healthy" homes. Allergy, 1994b. 49(10): p. 866-70. https://dx.doi.org/10.1111/j.1398-9995.1994.tb00789.x.
41. Niven, R., et al., Attempting to control mite allergens with mechanical ventilation and dehumidification in British houses. J Allergy Clin Immunol, 1999. 103(5 Pt 1): p. 756-62. https://dx.doi.org/10.1016/s0091-6749(99)70416-1.
42. Crane, J., et al., A pilot study of the effect of mechanical ventilation and heat exchange on house-dust mites and Der p 1 in New Zealand homes. Allergy, 1998. 53(8): p. 755-62. https://dx.doi.org/10.1111/j.1398-9995.1998.tb03971.x.
43. Fletcher, A.M., et al., Reduction in humidity as a method of controlling mites and mite allergens: the use of mechanical ventilation in British domestic dwellings. Clin Exp Allergy, 1996. 26(9): p. 1051-6. https://dx.doi.org/10.1111/j.1365-2222.1996.tb00643.x.
44. Aldous, M.B., et al., Evaporative cooling and other home factors and lower respiratory tract illness during the first year of life. Group Health Medical Associates. Am J Epidemiol, 1996. 143(5): p. 423-30. https://dx.doi.org/10.1093/oxfordjournals.aje.a008762.
45. Prasad, C., et al., Effect of evaporative coolers on skin test reactivity to dust mites and molds in a desert environment. Allergy Asthma Proc, 2009. 30(6): p. 624-7. https://dx.doi.org/0.2500/aap.2009.30.3290.
47. Etzel, R.A., et al., Acute pulmonary hemorrhage in infants associated with exposure to Stachybotrys atra and other fungi. Arch Pediatr Adolesc Med, 1998. 152(8): p. 757-62. https://dx.doi.org/10.1001/archpedi.152.8.757.
49. Mudarri, D. and W.J. Fisk, Public health and economic impact of dampness and mold. Indoor Air, 2007. 17(3): p. 226-235. https://dx.doi.org/10.1111/j.1600-0668.2007.00474.x.
50. Mudarri, D.H., Valuing the Economic Costs of Allergic Rhinitis, Acute Bronchitis, and Asthma from Exposure to Indoor Dampness and Mold in the US. J Environ Public Health, 2016. 2016: p. 2386596. https://dx.doi.org/10.1155/2016/2386596.